How to Track Coronavirus in Your APCD
States will be looking to their all-payer claims databases (APCDs) to gain a better understanding of the impact of the coronavirus pandemic. This blog post will offer suggestions on how to tap into APCDs to see trends in related healthcare utilization and cost.
What’s the difference between SARS-CoV-2 and COVID-19?
SARS-CoV-2 (short for Severe Acute Respiratory Syndrome Coronavirus 2) is the name of the virus that causes COVID-19 (short for Coronavirus Disease 2019).
How do I find SARS-CoV-2 and COVID-19 in my data?
You may find claims for diagnostic testing and treatment. SARS-CoV-2 infections cause a range of illness, from little to no symptoms, to those affected being severely ill and even dying. Symptoms can include fever, cough, and shortness of breath. The condition can progress to lower respiratory infection, bronchitis, pneumonia, and even acute respiratory distress syndrome.
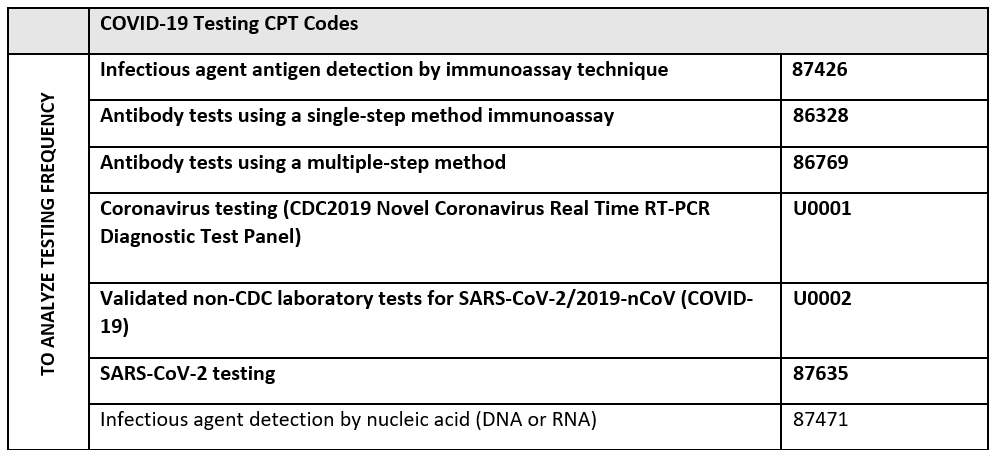
Testing
As of June 26, 2020, the AMA Current Procedural Terminology (CPT®) Editorial Panel has adopted a new CPT code to report antigen testing of patients suspected of SARS-CoV-2 infection (87426). Effective March 13, 2020, the AMA released a new CPT code for SARS-CoV-2 testing: 87635 Infectious agent detection by nucleic acid (DNA or RNA); severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]), amplified probe technique. Note that this is a more specific code under the existing “parent” code of 87471 Infectious agent detection by nucleic acid (DNA or RNA), which may be used when testing for any infectious agent, including COVID-19.
In addition, the Centers for Medicare & Medicaid Services (CMS) developed two new lab testing codes.
- U0001 will be reported for coronavirus testing using the Centers for Disease Control and Prevention (CDC) 2019 Novel Coronavirus Real Time RT-PCR Diagnostic Test Panel.
- U0002 will be reported for validated non-CDC laboratory tests for SARS-CoV-2/2019-nCoV (COVID-19).
The Medicare claims processing system will be able to accept this code on April 1, 2020 for dates of service on or after February 4, 2020. It is expected that other payers also will use these codes to support standardized billing and data analysis.
Similar to influenza, there is no code for swabbing for COVID-19. However, providers can report the specimen collection code 99000.
Diagnosis
The Centers for Disease Control and Prevention (CDC) recently released official diagnosis coding guidance for health care encounters and deaths related to COVID-19. A new diagnosis code specific to COVID-19, U07.1, will be effective April 1, 2020 as a revision of ICD-10-CM. The CDC said the unprecedented off-cycle update is due to the “urgent need to capture the reporting of this condition in our nation’s claims and surveillance data.”
For COVID related care prior to April 1, the CDC recommends using B97.29, Other coronavirus as the cause of diseases classified elsewhere in conjunction with the code for the reason for the encounter (e.g. pneumonia, acute bronchitis).
The CDC recommends only using the additional B97.29 code for confirmed cases of COVID-19. Suspected, possible or probable cases of COVID-19 are to be reported only with codes explaining the reason for the encounter.
Given this guidance and limited testing capacity, analysts should review care related to the diagnosis codes below with and without the B97.29 code to better understand care potentially related to COVID-19.
ICD-10 Diagnosis Codes to Explore*:
- Cough, R05
- Fever, unspecified R50.9
- Shortness of breath, R06.02
- Pneumonia, J12.89, Other viral pneumonia
- Acute Bronchitis, J20.8
- Bronchitis, Not Otherwise Specified, J40,
- Lower Respiratory Infection, J22
- Respiratory infection, Not Otherwise Specified, J98.8
- ARDS due to COVID-19, J80
*NOTES: As noted above, diagnosis codes should be analyzed with and without B97.29, Other coronavirus as the cause of diseases classified elsewhere. Some patients may be more likely to seek medical care for minor coughs and fevers that are unrelated. CDC has advised against coding COVID-19 as B34.2, Coronavirus infection, unspecified because the cases have consistently been respiratory in nature and therefore the site should not be classified as unspecified.
States may also be interested in better understanding residents who were exposed to COVID-19 but did not need care. The ICD-10 codes below can support this analysis.
Exposure to person(s) with confirmed COVID-19: Z20.828, Contact with and (suspected) exposure to other viral communicable diseases
Possible exposure to COVID-19, ruled out: Z20.818, Contact with and (suspected) exposure to other viral communicable diseases
Utilization
Inpatient Care: Providers report increased rates of emergency room visits and inpatient stays, including increased use of intensive care and ventilators.
CPT Codes to Explore:
- Hospital inpatient initial care: 99221, 99222, 99223
- Hospital inpatient subsequent care: 99231, 99232, 99233
- Hospital observation initial care: 99218, 99219, 99220
- Hospital observation subsequent care: 99224, 99225, 99226
- Hospital inpatient initial consult care: 99251, 99252, 99253, 99254, 99255
- Hospital admit/discharge same date care: 99234, 99235, 99236
- Outpatient established office care 99211, 99212, 99213, 99214, 99215
- Outpatient, new to office care: 99201, 99202, 99203, 99204, 99205
- Outpatient consult care: 99241, 99242, 99243, 99244, 99245
- Critical care: 99291 and 99292
- Hospital inpatient discharge codes: 99238, 99239
- Hospital observation discharge code: 99217
- Ventilator management 94656-94657
Outpatient Care: Rates of visits to physician offices, urgent care and telemedicine are also expected to increase.
CPT Codes to Explore*:
- Emergency department visits – 99283, 99284, 99285, 99281, 99282
- Urgent care – See note below*
- Office or outpatient visit for a new patient, 99201-99205
- Office or outpatient visit for an established patient, 99211-99215
- Non-physician telephone services, 98966, 98967, 98968
- Online assessment, mgmt services by non-physician, 98969
- Office or other outpatient consultations, 99241-99245
- Prolonged Service Office Visit, 99354-99355
- Prolonged Service Office Visit, 99358, 99359
- Telephone Evaluation and Management, 99441-43, G2010
- Non-face-to-face on-line Medical Evaluation, 99444
- Clinic visit, all-inclusive (FQHC), T1015
*Note: Urgent cares not associated with a health system bill on a professional claim and use the same codes as a physician office (e.g. 99202- 99205 and 99211-99215) often with an urgent care place of service code of 20. Urgent cares associated with a health system bill on the institutional health care claim with the revenue code 0456.
Concerned about capacity and disease transmission, some providers are rescheduling elective services and procedures. Therefore, there may also be decreases in common elective or non-urgent procedures such as joint replacements. We will explore this topic more in a future post.
Below is a list of codes commonly used to support analyses related to COVID-19. Codes in bold type were recently developed specifically for this purpose.
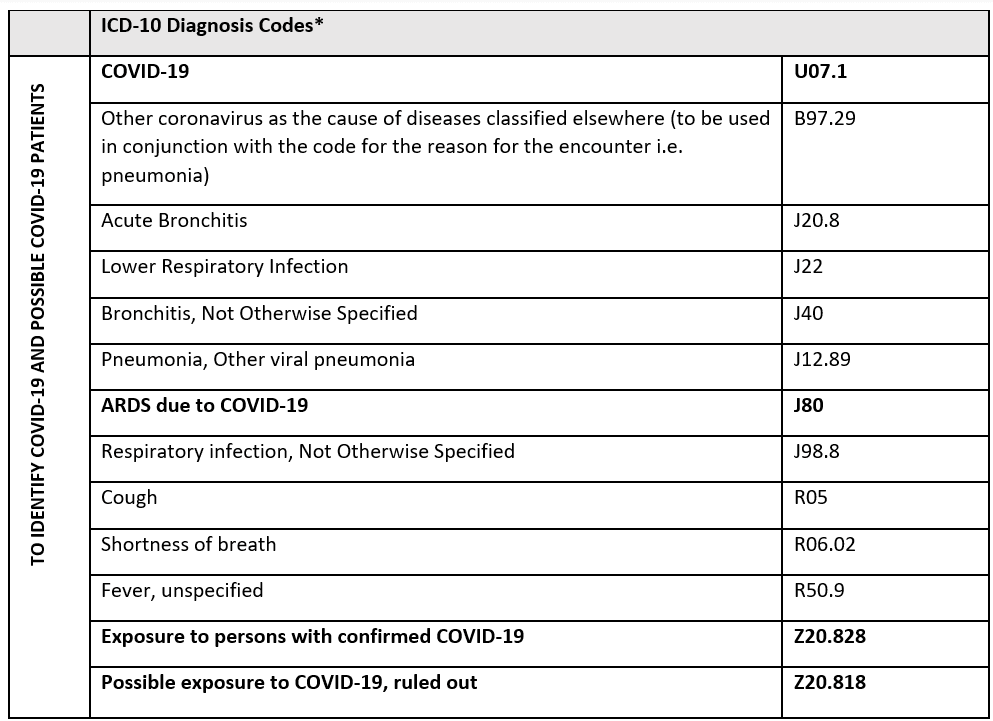

*The CDC recommends using U07.1 and using the additional B97.29 code only for confirmed cases of COVID-19. Suspected, possible or probable cases of COVID-19 are to be reported only with codes explaining the reason for the encounter. Given this guidance and limited testing capacity, analysts should review care related to the diagnosis codes below with and without the B97.29 code to better understand care potentially related to COVID-19.
For more information or assistance performing these analyses, contact Mary Jo Condon at [email protected]
Updated June 30, 2020.

