Thursday Thoughts with Douglas McCarthy, President of Issues Research, Inc.
In this latest installment of our Thursday Thoughts series, FHC Senior Health Care Data/Policy Consultant Jonathan Mathieu talked to Douglas McCarthy, M.B.A, president of Issues Research, Inc., in Durango, Colorado.

Mr. McCarthy has more than 30 years of experience in the public, private, and nonprofit sectors and has consulted on projects for corporations, foundations, and universities. As senior research advisor to the Commonwealth Fund, he conducts case study research examining best practices and innovations in health care delivery and cost containment. The Fund recently published reports that he authored examining how states establish and benefit from all-payer claims databases (APCDs). Mr. McCarthy previously worked at the Institute for Healthcare Improvement and UnitedHealth Group’s Center for Health Care Policy and Evaluation. He serves on the boards of Colorado’s Center for Improving Value in Health Care and the Peak Health Alliance.
Jonathan Mathieu: What’s surprised you the most in the past 6 months?
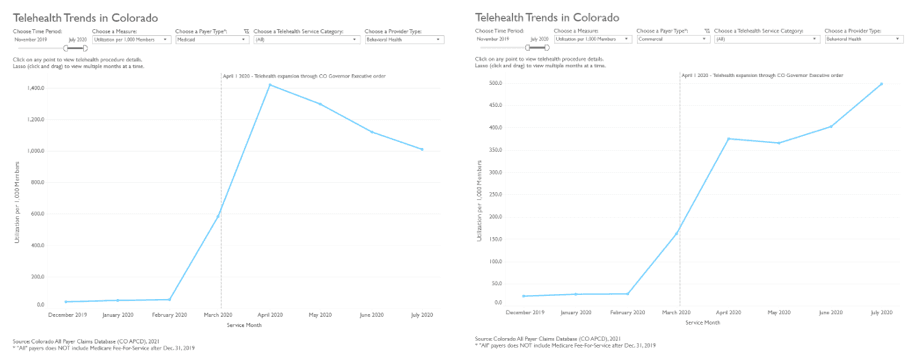
Douglas McCarthy: I have been pleasantly surprised to see rapid analyses of health insurance claims data tracking the impact of the COVID-19 pandemic. For example, the Center for Improving Value in Health Care (Colorado’s APCD administrator) published an interactive tool showing how telehealth was used before and during the pandemic. In my past work tracking health system performance, we typically saw a two-year lag in measures that relied on Medicare claims data. Now we’re seeing analyses of data that are less than six months old. This timelier reporting makes the data much more relevant.
JM: What’s been the data that’s most guided your work in the past 6 months?
DM: I’m going to lengthen the timeframe of your question to talk about how a health care purchasing cooperative in Colorado, Peak Health Alliance, used data from the Colorado APCD to assess where residents are getting health care and how much it costs. We used this data in discussions with community stakeholders to identify opportunities for making health care more affordable in western Colorado, where insurance premiums are among the highest in the nation. Developing a common understanding of the situation aided our efforts to enlist the cooperation of health care providers to participate in an innovative health insurance plan that reduced premiums by up to 35 percent.
JM: What’s the most interesting statistic you’ve seen in the past 6 months?
DM: The interactive tool that I mentioned earlier reveals some fascinating trends in the use of telehealth in Colorado. For example, while the overall use of telehealth peaked in April 2020 and then declined in the following months, its use for behavioral health continued to increase for commercially insured and Medicare Advantage patients through the summer. Behavioral telehealth was used most intensively among Medicaid-insured patients—at a rate three times greater than among commercially insured patients at the April peak. These data show how payers responded nimbly to the need for services and suggest that some types of telehealth may have staying power throughout and after the pandemic.
JM: What have you learned about doing your work better, faster that should be shared and preserved?
DM: Like many people who telework (I live in southwest Colorado), I have benefited from the shift to virtual meetings during COVID that has expanded the opportunity for rapid learning and tracking developments in the industry (such as innovations in the use of telehealth). Video calls have now become an accepted mode of business communication, which makes it possible to streamline the process of conducting case studies using virtual site visits. Granted we’re all getting Zoom fatigue, so we’ll have to find a happy balance of in-person, virtual, and blended formats that allows us to reap the best of each going forward.
JM: What should we be measuring 6 months from now?
DM: We need to use our collective data resources to assess the extent and impact of foregone care during the pandemic, both to gauge its impact and to identify and address critical unmet needs. This analysis may also offer insight on where it’s possible to reduce low-value services without adversely affecting population health. That kind of insight will require sophisticated analytic approaches combining data from multiple sources such as claims, surveys, and vital records. Ultimately, such an assessment should help the country better prepare for the next public health crisis when it comes.
___________________________________________
Interested in hearing more about how health data experts from around the country are learning from and working within a COVID-19 world? Check out the other installments in our series, such as our conversation with Director of Strategy and Analytics at Virginia Health Information, Kyle Russel, discussing interconnectedness, real-time data, and new trends in data.
